The Ultimate Guide to Prebiotic Prescription
What Are Prebiotics and Why Do They Matter in Practice?
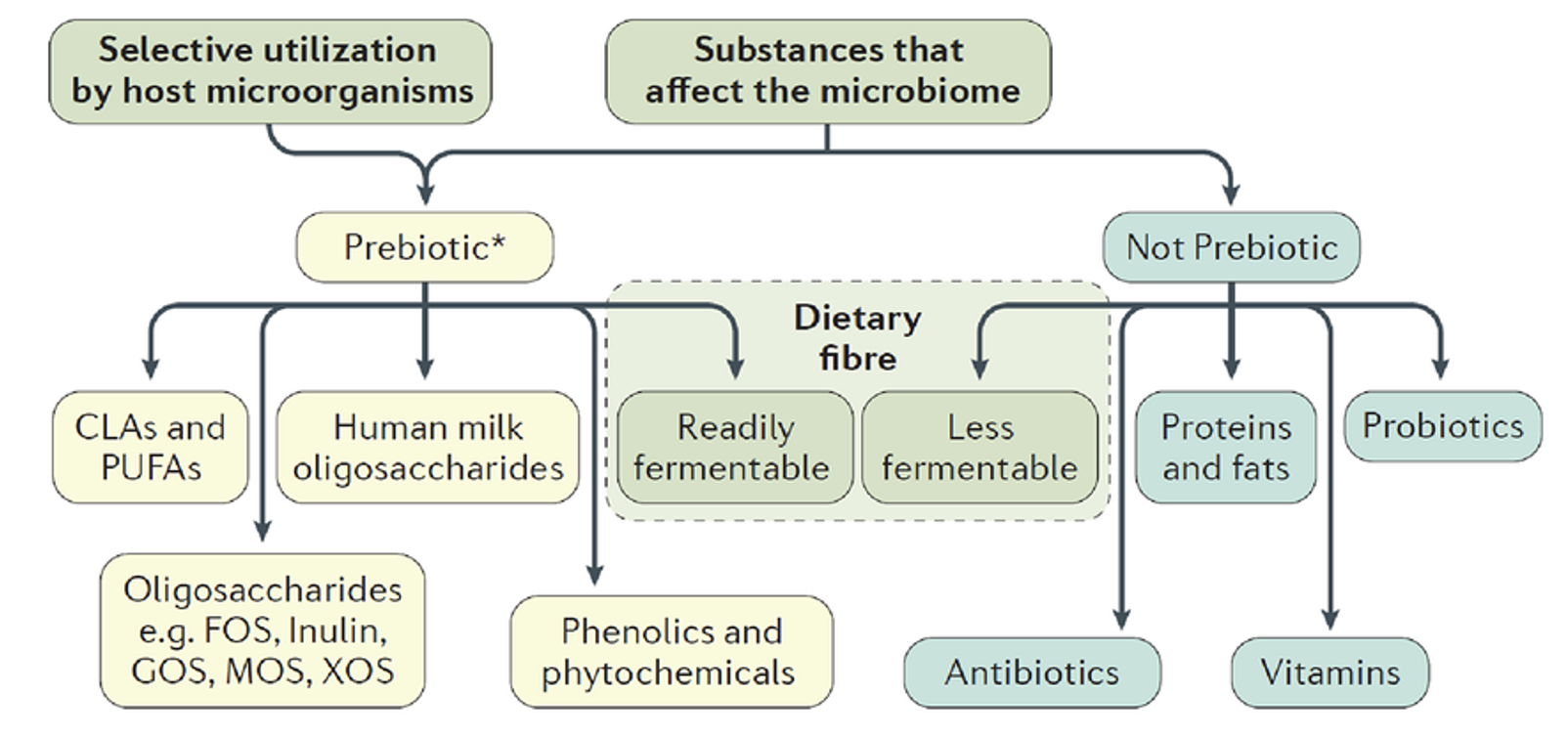
Prebiotics are far more than just “fibre.” They are the unsung heroes of gut health, specialized, fermentable substrates that selectively feed and nurture beneficial microbes within the intestinal ecosystem. For practitioners, this distinction is critical: while all fibres can influence digestion, only prebiotics have been clinically defined to stimulate the growth of health-promoting bacteria and enhance host wellbeing.
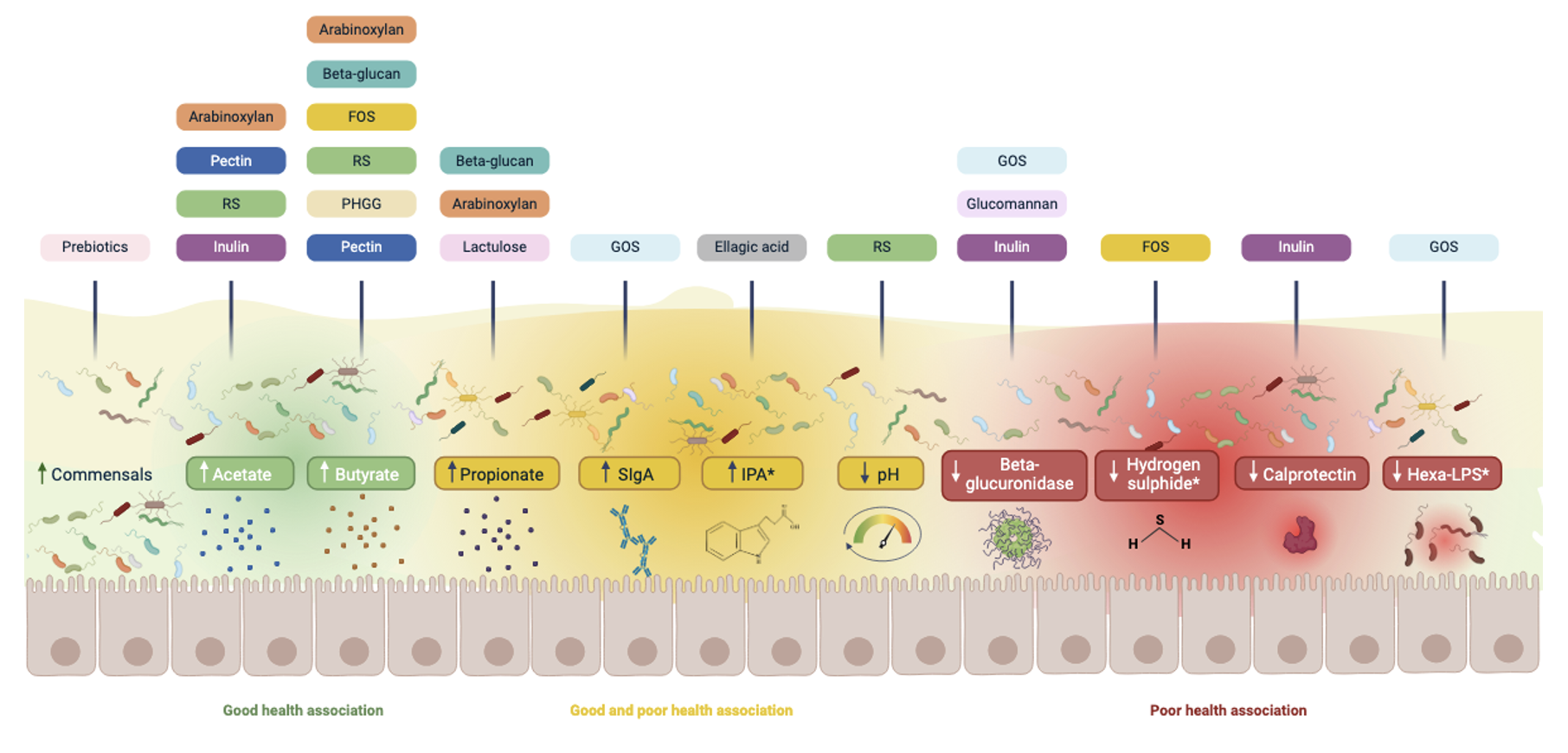
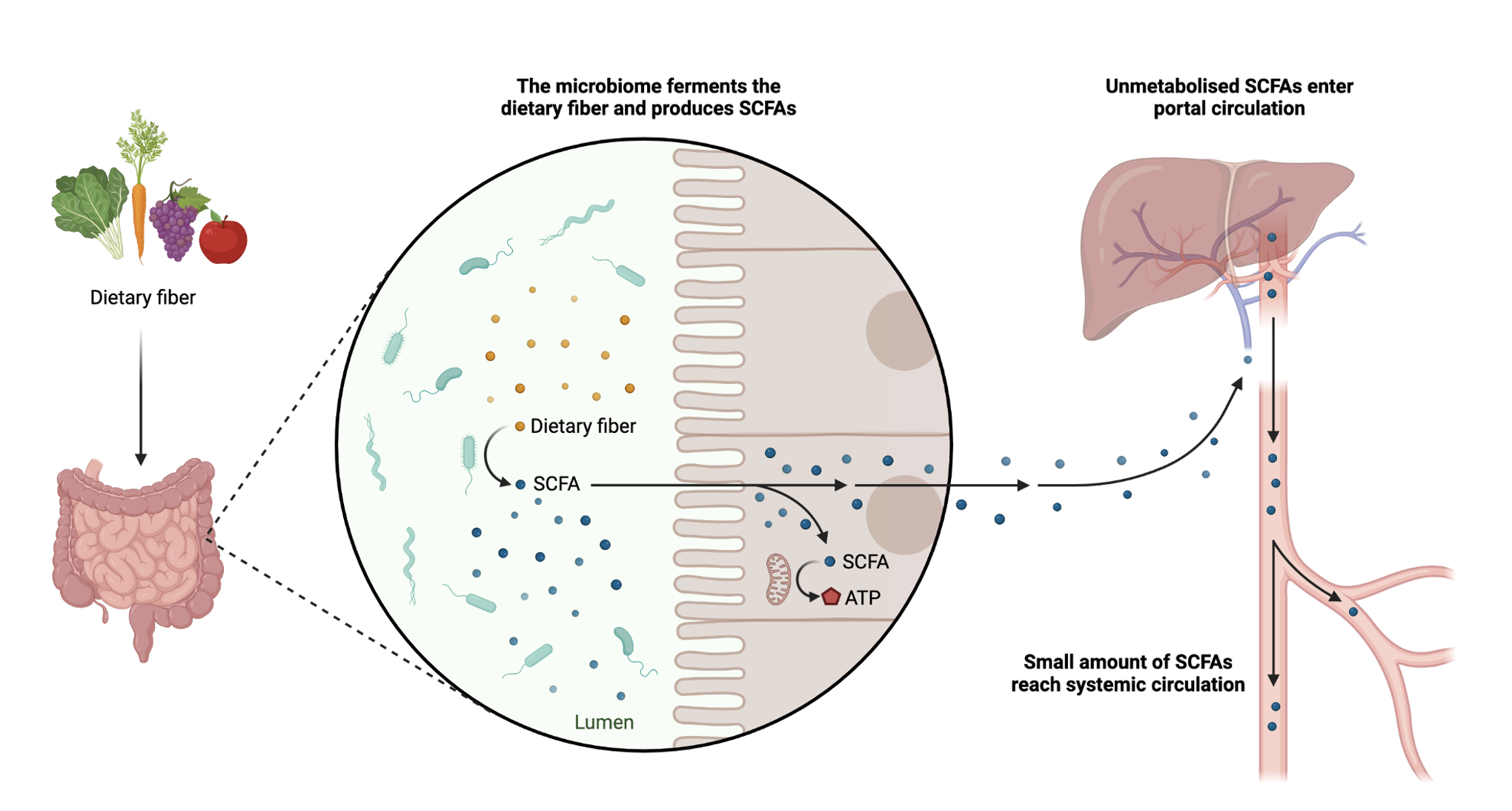
Here’s the fun part: humans don’t actually digest prebiotics. Instead, we outsource this job to our gut microbiome, who transform them into powerful metabolites like short-chain fatty acids (SCFAs). Think of SCFAs as the molecular currency of gut health, they fuel colonocytes, regulate immune function, improve insulin sensitivity, and even cross the blood–brain barrier to influence mood and cognition.
Clinical Pearl:
A single gram of prebiotic fibre can yield millimoles of butyrate, one of the most potent anti-inflammatory molecules produced in the gut. That’s a therapeutic return on investment few interventions can match.
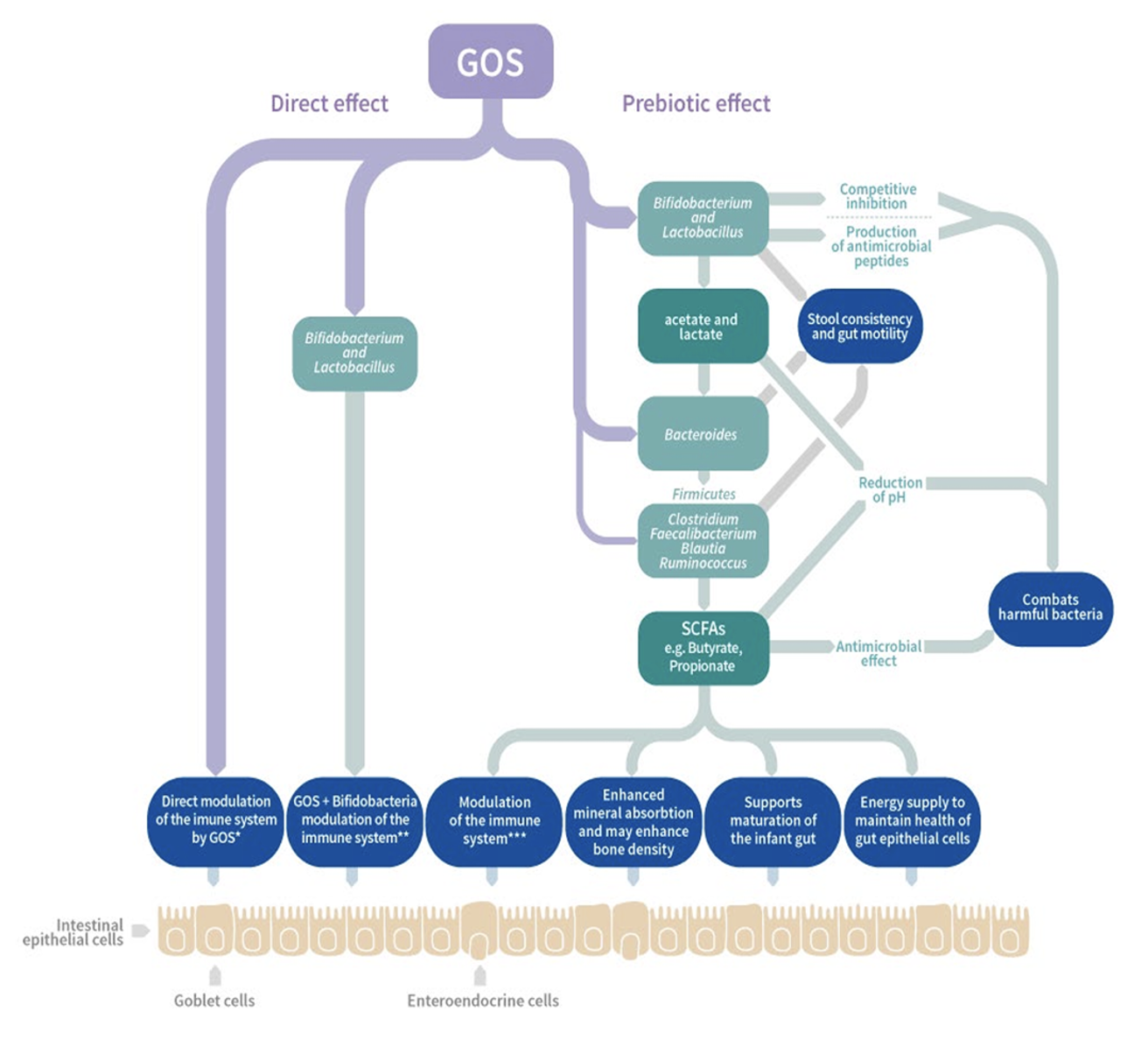
Another fascinating insight? Prebiotics can be as selective as antibiotics, but in reverse. Instead of suppressing broad swathes of bacteria, they preferentially feed keystone species like Bifidobacterium and Akkermansia, shaping the microbial community toward resilience and diversity. For instance, galacto-oligosaccharides (GOS) have a documented bifidogenic effect, while resistant starch preferentially boosts butyrate producers.
For clinicians, this means prebiotic prescription isn’t about “more fibre” in general, it’s about choosing the right tool for the right patient, and layering interventions to encourage a diverse, balanced microbiome. The growing body of research consistently shows that a low dose of multiple prebiotics, titrated slowly over time, yields superior outcomes compared to a high dose of any single compound.
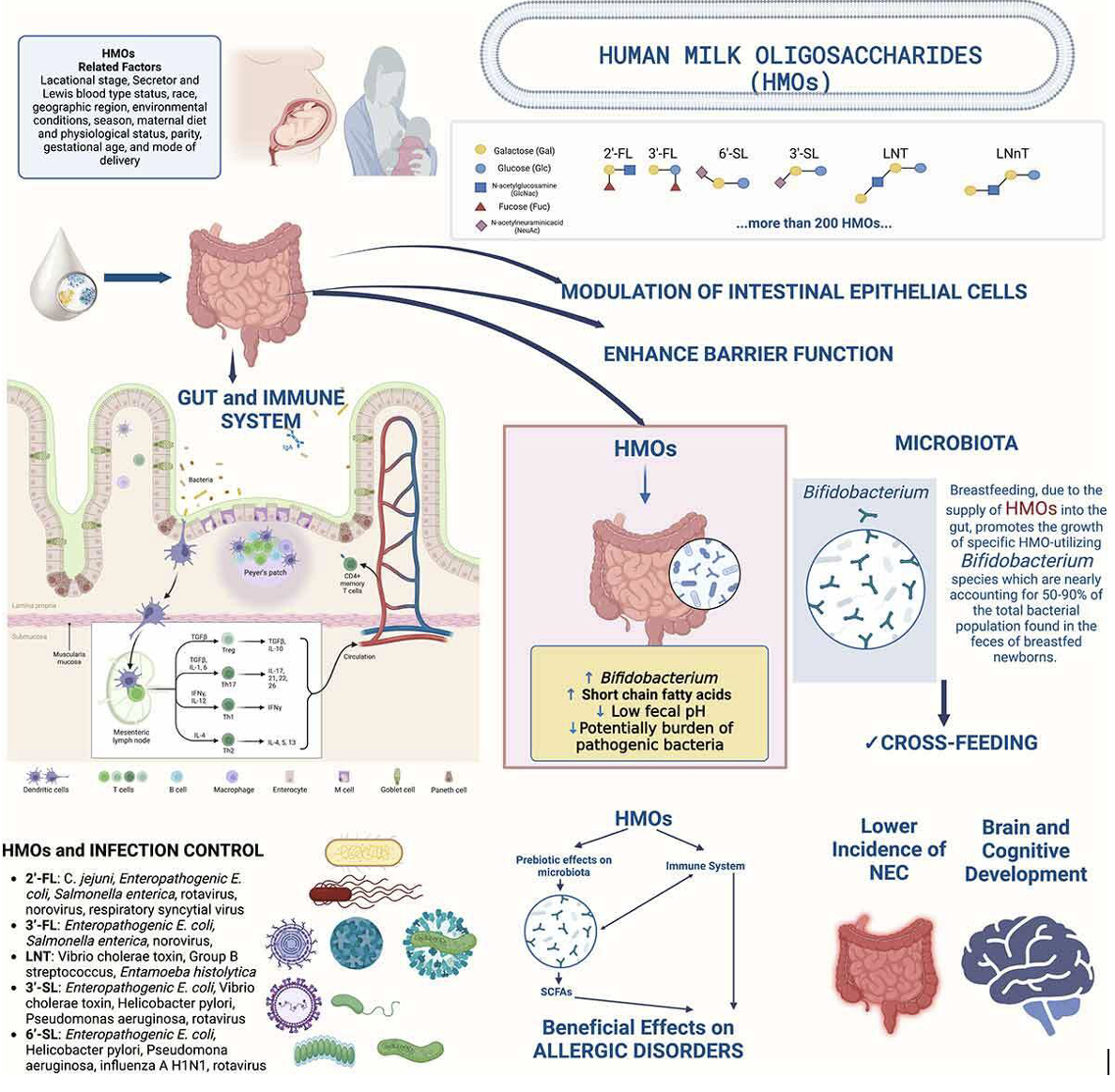
And here’s a fun fact to share with patients: our first exposure to prebiotics happens at birth. Human milk oligosaccharides (HMOs) are nature’s original prebiotic, designed to feed infant bifidobacteria rather than the infant itself. This evolutionary design underscores the profound role prebiotics play in shaping health from the very beginning of life.
The clinical application of prebiotics extends far beyond gut comfort. Emerging research shows that specific substrates can influence systemic pathways, from metabolic regulation to immune modulation. By selectively nourishing beneficial taxa, prebiotics drive the production of short-chain fatty acids, reduce pro-inflammatory mediators, and support barrier integrity. What makes this field particularly exciting for practitioners is the capacity to match targeted prebiotic interventions with defined clinical outcomes, moving us closer to precision nutrition in everyday practice.
Different Prebiotics Feed Different Gut Microbes
One of the most exciting things about prebiotics is their specificity. Just like certain nutrients target particular tissues in the body, different prebiotics preferentially feed different microbial species in the gut. This isn’t a case of “fibre is fibre.” It’s a case of matching the substrate to the species, and that’s where clinical precision comes alive.
For example, GOS (galacto-oligosaccharides) have a well-documented bifidogenic effect, reliably expanding Bifidobacterium populations. Resistant starch, on the other hand, is the favorite meal of butyrate-producing powerhouses like Faecalibacterium prausnitzii and Roseburia. Meanwhile, PHGG offers a steady, gentle fermentation that benefits a wide range of taxa without overwhelming sensitive guts. When we think about prescribing prebiotics, it’s less about one “magic bullet” and more about building a symbiotic ecosystem.
Clinical Pearl:
Instead of pushing a patient onto a high dose of a single prebiotic, consider layering small doses of several types. This supports multiple keystone species simultaneously, creating diversity and resilience without overwhelming the gut.
New research has shown microbes don’t live in isolation, they share food. This process, known as cross-feeding, means the by-products of one species become fuel for another. For instance, bifidobacteria fed by GOS produce acetate, which butyrate producers like Roseburia then use to generate butyrate.
Fun Fact: A single gram of resistant starch can shift fermentation downstream to the colon, where butyrate production peaks, making it one of the most efficient ways to fuel colonocytes and support gut barrier integrity.
When you combine prebiotics strategically, you’re not just feeding bacteria, you’re orchestrating an entire microbial community. Diversity begets resilience, and resilience begets health. This is why the best approach isn’t “maximum dose” but rather “low and slow, layered and diverse.” Patients are more likely to tolerate the intervention, and the microbiome is more likely to flourish.
Clinical Pearl:
Prebiotic tolerance improves dramatically when doses are increased gradually. Start patients low, just a gram or two, and build over weeks. This reduces bloating and discomfort, increases compliance, and allows microbial populations to adapt sustainably.
In practice, this means thinking like an ecologist: which species need support, what substrates feed them, and how can we balance diversity while minimizing symptoms? When we get it right, prebiotics transform from “just fibre” into one of the most elegant clinical tools for restoring microbiome health.
PromOat® Beta-Glucan : A Prebiotic for Metabolic and Microbiome Health
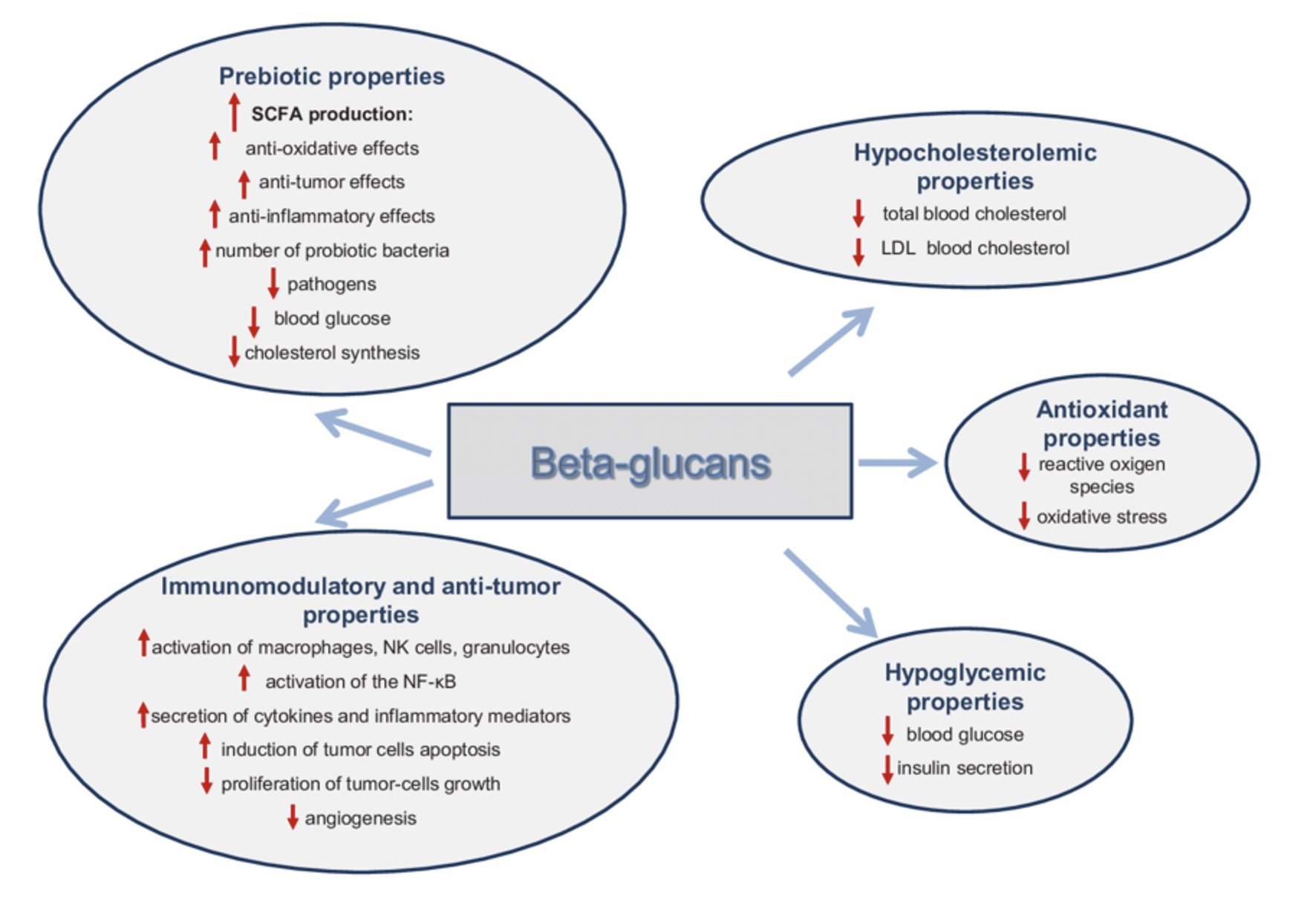
Beta-glucans are not your average fibre, they are biological modulators. Derived from oats, PromOat® delivers 29% beta-glucan that not only nourishes the microbiome but also directly interacts with the host’s immune system.
Benefits to the Microbiome: Beta-glucan selectively boosts bifidobacteria populations while also increasing SCFA output, especially acetate. This creates downstream benefits for metabolic and immune regulation.
Fun Fact: Oat beta-glucans have been shown to “talk” to immune cells via Dectin-1 receptors on macrophages, meaning they work on both sides of the gut–immune axis.
Dosage Range: 3–7 g/day has been clinically validated for cholesterol and glycaemic improvements.
Scientific Findings: A wealth of RCTs demonstrate reductions in LDL cholesterol, improved glycaemic control, and enhanced satiety.
Clinical Pearl: Ideal for patients with metabolic syndrome, cardiovascular risk, or inflammatory load. PromOat® makes a beautiful base prebiotic, gentle enough for most patients, but clinically potent in systemic outcomes.
NuBana™ Green Banana Flour: Resistant Starch for Butyrate Production
NuBana™ Green Banana Flour contains 60% resistant starch which is often underappreciated in clinical practice, yet it is one of the most effective prebiotics for butyrate production.
Benefits to the Microbiome: Resistant starch type 2 feeds butyrogenic bacteria such as Roseburia and Faecalibacterium prausnitzii, strengthening gut barrier integrity and reducing inflammation.
Fun Fact: In many traditional diets (think Pacific islands or Africa), green bananas have been a staple for centuries, delivering natural prebiotics long before we had the science to name them.
Dosage Range: 5–15 g/day, titrated slowly to reduce bloating.
Scientific Findings: Clinical trials show improved insulin sensitivity, reduced postprandial glucose, and enhanced satiety. Butyrate production rises significantly within weeks of use.
Clinical Pearl:
Excellent for patients with inflammatory bowel conditions, metabolic dysfunction, or those requiring colonic repair. Always start low and go slow, the fermentative power of resistant starch can be intense at higher doses.
Bimuno® GOS (Galacto-oligosaccharides): The Clinician’s Favorite for bifidobacteria
If there were a “poster child” for prebiotics, GOS would be it. Widely studied and well tolerated, Bimuno® GOS is one of the most clinician-friendly tools for reshaping the microbiome.
Benefits to the Microbiome: Selectively stimulates bifidobacteria, reduces populations of pathogenic bacteria, and improves microbial balance.
Fun Fact: A clinical trial found that GOS supplementation in stressed students reduced cortisol awakening response and improved resilience!
Dosage Range: 2–6 g/day.
Scientific Findings: Proven in IBS patients to reduce bloating and pain, supports immune balance, and improves traveller’s diarrhoea outcomes.
Clinical Pearl:
The superior tolerability of β-GOS over α-GOS is one reason Bimuno® has become the “gold-standard” GOS supplement, it delivers consistent bifidogenic benefits without the high rates of GI side effects seen with α-GOS.
2’-Fucosyllactose (2’-FL): Harnessing the Power of Human Milk Oligosaccharides
Nature’s original prebiotic, an HMO, designed by evolution to nourish the infant microbiome. 2’-FL has now been harnessed for adults and children alike, with profound implications.
Benefits to the Microbiome: Promotes the growth of Bifidobacterium infantis and other beneficial infant-type strains, enhances gut barrier integrity, and modulates immune responses.
Fun Fact: Infants don’t digest HMOs like 2’-FL; instead, these sugars pass through the small intestine intact, deliberately feeding beneficial microbes in the colon. It’s the perfect example of host–microbe co-evolution.
Dosage Range: 1–2 g/day.
Scientific Findings: Reduces incidence of infections in infants, modulates allergy risk, and early research suggests benefits in adults with immune dysregulation or dysbiosis.
Clinical Pearl:
Brilliant for paediatric cases, post-antibiotic recovery, or immune-sensitive patients. If a patient has recurrent infections, 2’-FL deserves a place in your toolkit.
Sunfibre® (Partially Hydrolyzed Guar Gum, PHGG): A Gentle, FODMAP-Friendly Prebiotic for Sensitive Patients
PHGG is the workhorse prebiotic, gentle, versatile, and highly tolerable across a wide range of patients.
Benefits to the Microbiome: Steady fermentation enhances bifidobacteria, increases SCFA production, and supports regular bowel function.
Fun Fact: Unlike many fibres, PHGG is FODMAP-friendly at lower doses, making it one of the only prebiotics patients with IBS can tolerate from day one.
Dosage Range: 3–10 g/day.
Scientific Findings: Clinical trials show PHGG normalizes bowel movements in both IBS-C and IBS-D, improves microbial diversity, and reduces GI discomfort.
Clinical Pearl:
Think of PHGG as the “gateway prebiotic.” If patients have had bad experiences with fermentable fibres, PHGG is often the safest and most effective reintroduction.
Measuring the Microbiome: The Key to Personalising Prebiotic Prescription
It’s one thing to know that prebiotics feed microbes. It’s another to know which microbes your patient actually has. This is where microbiome testing becomes a powerful clinical tool. By identifying the relative abundance of bacterial species, we can move from a “shotgun” approach to a precision-guided prescription.
For instance, if testing reveals a depletion of butyrate producers such as Faecalibacterium prausnitzii or Roseburia, you might prioritise resistant starch (NuBana™) or oat beta-glucan (PromOat®). Conversely, if bifidobacteria are low, GOS (Bimuno®) or HMOs (2’-FL) make strategic sense. And if testing shows global diversity loss, layering multiple prebiotics in low doses can help rebuild ecological resilience.
Clinical Pearl: Microbiome testing doesn’t just guide what to prescribe, it also informs what not to prescribe. For example, if a patient has overgrowth of gas-producing species, a cautious approach to rapidly fermenting fibres like inulin or FOS may prevent symptom flare-ups.
Measuring the microbiome also offers patients a tangible way to see progress. Many people with gut issues feel frustrated when symptoms fluctuate. Showing them before-and-after shifts in bacterial populations or SCFA potential provides validation that their hard work and your prescription, is making a measurable impact.
Microbiome testing provides invaluable insights into the diversity and composition of your patient’s gut microbiome, allowing you to make more precise decisions when prescribing prebiotics. Understanding which microbial species are abundant or lacking helps you tailor prebiotic supplementation to each patient’s unique microbiome, optimising therapeutic outcomes.
By integrating microbiome testing, such as the MetaXplore GI Plus from Co-Biome by Microba, into your clinical practice, you can personalise prebiotic interventions based on robust, data-driven insights. This approach ensures that you maximize the therapeutic potential of prebiotics in improving gut health and addressing your patients’ specific clinical needs.
Practical Clinical Application: How to Prescribe and Combine Prebiotics
Prescribing prebiotics is both an art and a science. On paper, we know which substrates feed which species. But in the clinic, success lies in how we introduce, combine, and titrate these interventions to match the patient’s unique microbiome and tolerance.
The golden rule? Low and slow. Many patients come to us after trying to “fix their gut” by jumping straight into large doses of fibre powders, only to end up bloated, crampy, and discouraged. Instead, begin with small, layered doses, often just 1–2 grams per day of a given prebiotic, and gradually increase as tolerance builds. Over time, microbial communities adapt, fermentative capacity improves, and patients enjoy greater comfort and compliance.
When it comes to prebiotics, diversity is key. Rather than choosing a single fibre and pushing the dose high, the evidence consistently shows that a low-dose, multi-prebiotic approach is the most effective way to encourage microbial resilience. Starting with a combination of substrates such as beta-glucan, resistant starch, GOS, 2’-FL, and PHGG provides fuel for different microbial groups right from the beginning, laying the foundation for balanced fermentation and broad-spectrum SCFA production.
The important part is how you prescribe them. Begin with a low dose of the combined prebiotics and allow time for the gut to adapt. By titrating slowly upwards, patients minimise unwanted symptoms like bloating or gas, while giving their microbiome the chance to expand and stabilise. Over time, as tolerance improves, the dose can be increased to achieve stronger therapeutic effects.
Clinical Pearl: Combining multiple prebiotics at the outset helps prevent “overfeeding” one microbial group while neglecting others. Instead, you cultivate a diverse ecosystem, one that mirrors the natural variety seen in diets rich in whole plant foods.
Titration Tips
Start with a low daily serve that includes several different prebiotic fibres.
Increase gradually, usually every week or two, according to tolerance and clinical outcomes.
Emphasise consistency: daily intake is far more impactful than irregular, large doses.
Clinical Pearl: Bloating and gas during the early stages of prebiotic therapy aren’t always a bad sign, they can reflect microbial activity ramping up. Reassure patients that with careful titration, symptoms usually settle as the ecosystem stabilizes.
Introducing Biome Diversity
In my clinical practice, I prefer to use Biome Diversity as a foundation for prebiotic therapy, given its balanced blend of prebiotics that support multiple microbial pathways. To access Biome Diversity, join Vitally and Dr Brad Leech will review your request and prescribe Biome Diversity if appropriate.
Why a Low-Dose, Multi-Prebiotic Strategy Is Best for Microbiome Diversity
Prebiotics are not just about digestion; they are about rewiring the microbiome for resilience, diversity, and systemic health. As practitioners, we stand at the frontier of a therapeutic shift where feeding microbes becomes as essential as feeding patients. The evidence is clear: diversity matters. And the best way to cultivate diversity is not with a single, high-dose prebiotic, but with a low-dose, multi-prebiotic strategy introduced gradually over time.
By layering PromOat® Beta-Glucan, NuBana™ Green Banana Flour, Bimuno® GOS, 2’-Fucosyllactose, and Sunfibre® (PHGG), we target a wide spectrum of beneficial species, foster cross-feeding networks, and boost the production of short-chain fatty acids like butyrate, the true currency of gut health. This synergy doesn’t just improve stool form or reduce bloating; it modulates immunity, reduces inflammation, supports metabolic balance, and even influences mood and cognition.
So, as you guide patients through their gut health journey, remember this: prebiotics are not optional add-ons. They are foundational. When used thoughtfully, low dose, diverse, and sustained, they become one of the most elegant, evidence-based, and powerful tools in your clinical practice.
Dr Brad Leech
Brad is a PhD-qualified Clinical Nutritionist and Herbalist specialising in chronic autoimmune conditions and complex gastrointestinal disorders. He provides complete and personalised care to his patients using functional nutrition, integrative medicine and holistic wellness.